Most people treat headaches as a small inconvenience—something you solve with water, rest, or an over-the-counter painkiller. But migraine is not a normal headache. It is a neurological disorder that affects more than 1 billion people worldwide and can send even healthy adults into a dark room for hours.
Yet many people suffering from migraine don’t even realize it. They think they’re “just tired” or “stressed,” when in reality, their brain is experiencing electrical, vascular, and sensory disturbances that simple painkillers can’t fix.
Doctors emphasize that the key to treating migraine is recognizing it early. Here are the three clearest differences between a regular headache and a migraine—and why it matters.
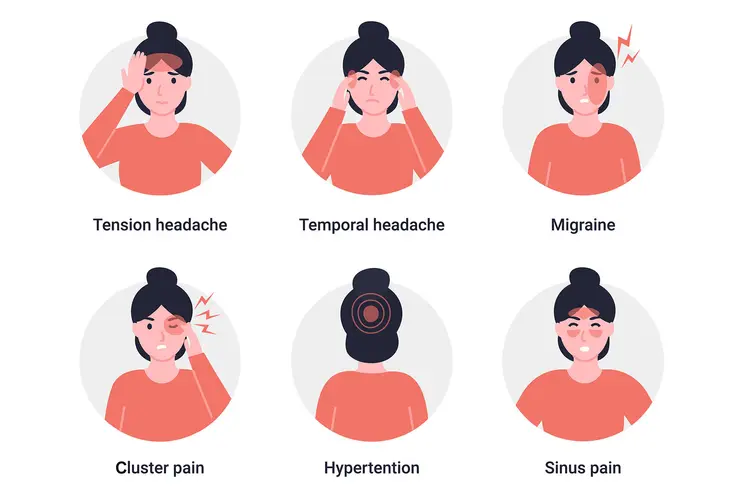
1. The Pain Quality Is Completely Different
A normal tension headache usually feels like:
-
A tight band around the forehead
-
Mild to moderate pressure
-
Discomfort that allows daily activities to continue
Migraine, however, produces a unique and often disabling pain that has these features:
● Throbbing or pulsating pain
People describe it as “a heartbeat inside the head,” “hammering,” or “pulsing.”
● Usually one-sided
About 60–70% of migraine attacks occur on one side of the head, although it can switch sides.
● Moderate to severe intensity
The pain is strong enough to interfere with work, conversation, and focus. Many individuals must lie down.
● Made worse by routine movement
Walking, bending, or turning the head often intensifies the pain. With a regular headache, movement doesn’t change much.
Doctors stress:
If the pain feels like pressure → probably a headache.
If it feels like your head is “pounding” or “expanding” → likely a migraine.
2. Migraine Comes With Additional Symptoms—Headache Does Not
This is the most important distinction.
A regular headache almost never comes with other major symptoms.
Migraine, on the other hand, is a multi-system attack involving the nervous system, digestive system, and senses.
Common migraine-related symptoms include:
● Nausea or vomiting
Up to 90% of migraine sufferers experience nausea during attacks.
● Sensitivity to light (photophobia)
Bright light becomes painful, forcing the person into a dark room.
● Sensitivity to sound (phonophobia)
Even small noises become overwhelming.
● Sensitivity to smell (osmophobia)
Perfume, food, or smoke can trigger discomfort.
● Blurred vision or difficulty focusing
● Extreme fatigue or weakness
● Neck stiffness or soreness
Migraine is essentially a whole-body neurological event, not just a pain in the head. Doctors say that if your “headache” forces you to lie down, close your eyes, turn off lights, or avoid noise, it is almost certainly a migraine.
3. The Body Often Gives Early Warning Signs Before Migraine—and Almost Never Before a Regular Headache
One of the most distinctive features of migraine is the presence of pre-attack warning signs, known as prodromes.
These can appear hours or even a day before the headache begins.
Common early signs include:
-
Sudden irritability or mood changes
-
Strong food cravings (especially sweets)
-
Stiff neck
-
Frequent yawning
-
Difficulty concentrating
-
Unusual tiredness
-
A sense of “something is coming”
Many patients describe it as their brain “shutting down” or becoming foggy before the pain starts.
Aura: The Most Recognizable Sign
About 25% of migraine patients experience aura—a temporary neurological disturbance that happens right before the pain phase.
Aura symptoms include:
-
Zigzag lines or flashing lights in vision
-
Blind spots
-
Tingling in hands or face
-
Difficulty speaking
-
Numbness
These signs rarely occur in a regular headache.
If you experience aura, doctors say the diagnosis is almost certainly migraine.
Why Understanding the Difference Matters
Many people with migraine do not receive proper treatment because they assume “it’s just a headache.” This leads to:
-
Overuse of painkillers
-
Worsening attacks
-
Lost productivity
-
Chronic migraine development
-
Increased risk of medication-overuse headaches
The earlier you identify migraine, the easier it is to control.
How Doctors Recommend Treating Migraine
Treatment focuses on speed, prevention, and lifestyle stability.
1. Treat Early
Take migraine-specific medication (like triptans or gepants) at the first sign of symptoms.
2. Identify Triggers
Common triggers include:
-
Stress
-
Hormonal fluctuations
-
Sleep irregularities
-
Strong smells
-
Alcohol (especially wine)
-
Skipping meals
-
Weather changes
A diary helps pinpoint your personal triggers.
3. Preventive Care
For frequent attacks (more than 4 per month), doctors may prescribe:
-
Preventive medications
-
Magnesium or riboflavin supplements
-
Botox (for chronic migraine)
-
CGRP monoclonal antibodies (new generation therapy)
4. Lifestyle Foundations
A consistent daily rhythm significantly reduces migraine frequency:
-
Regular sleep schedule
-
Balanced meals
-
Hydration
-
Moderate exercise
-
Avoiding sensory overload
Migraine brains are sensitive—stability helps.
Final Thoughts: Migraine Isn’t “Just a Headache”
Migraine affects your brain, senses, energy, mood, and daily functioning.
It has distinctive pain patterns, specific symptoms, and predictable warning signs that clearly separate it from an ordinary headache.
Understanding these differences not only gives you clarity—it ensures you get the right treatment at the right time.